The gut microbiome, our healthy gut bacteria, is a fascinating collection of various bacteria unique to each individual and plays a very important role in the body (1). We talked more in depth about the microbiome, the central and intrinsic nervous system, how the gut and brain cross connect, as well as one of the neurotransmitters in communication with the microbiome (serotonin) in the previously blogs “Your Gut: The Second Brain” and “The Gut-Brain Axis: Serotonin”. If you have not had a chance to read those yet, be sure to go back to get some basics for the topic on the gut-brain axis. This blog is going to continue to talk about another type of neuro-transporter, catecholamine, and its role in this incredible interaction and within the body.
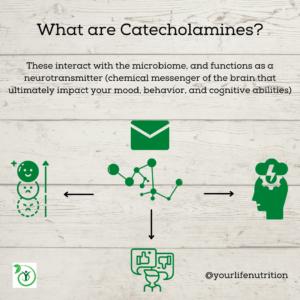
Catecholamine, just like serotonin, is one of five biogenic substances that contains at least one amine group, interacts with the microbiome, and functions as a neurotransmitter (1). This sounds pretty intimidating, but it simply means catecholamines can send chemical messages to the brain that ultimately impact your mood, behavior, and cognitive abilities (1). This means that the food you eat has a secondary impact on your mood (1). If the gut microbiome is not happy, these neurotransmitters that impact mood will not be made or cannot function properly, therefore impacting your gut health and cognitive health (1).
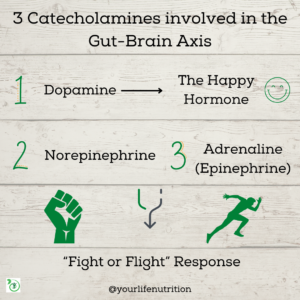
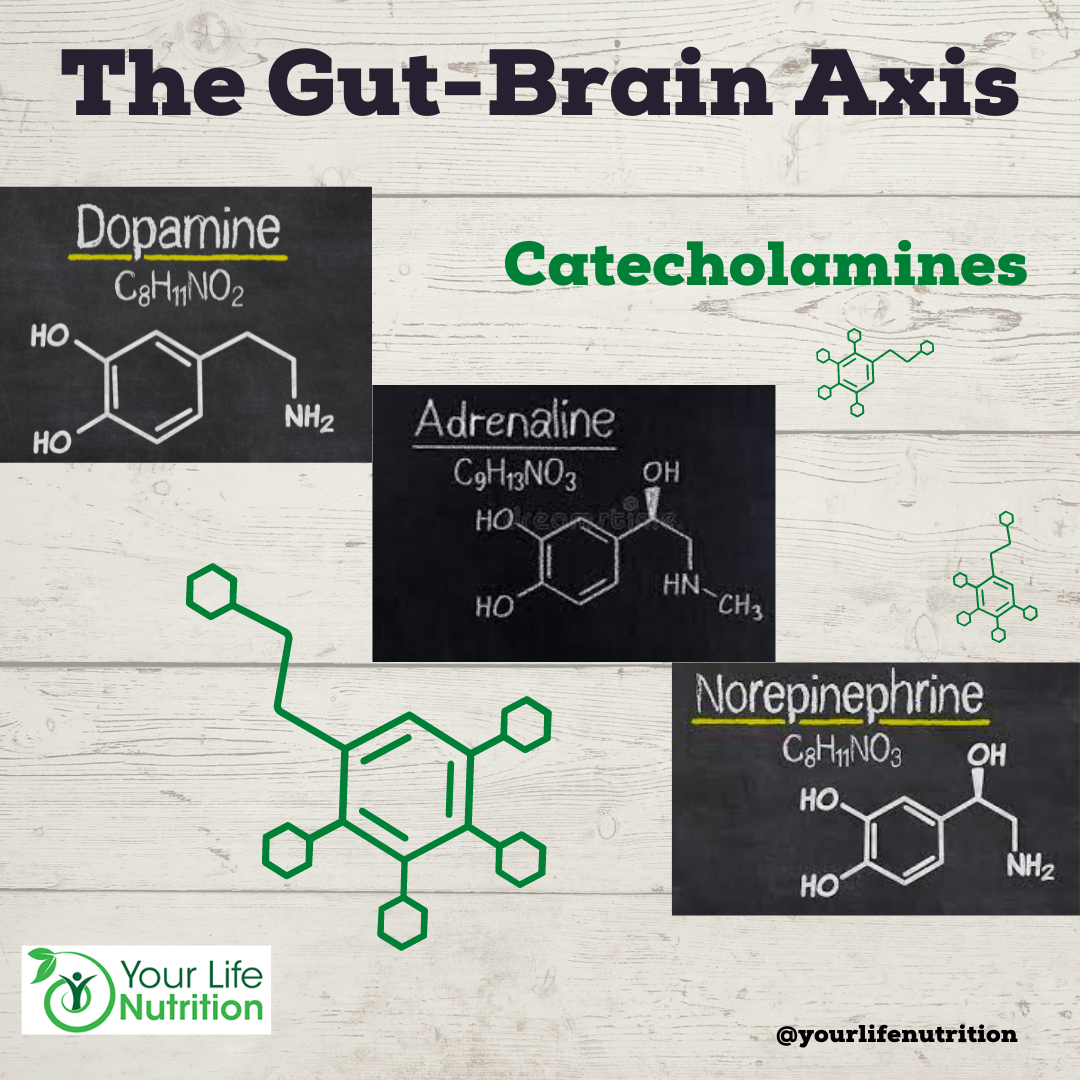
There are different types of catecholamines that are related to the brain-gut axis, norepinephrine, epinephrine (also referred to as adrenaline), and dopamine (1). Norepinephrine and epinephrine signal the “fight or flight” response while dopamine is a central catecholamine which acts as the “reward” or “pleasure” signal from a direct stimulation of the GI tract (2). These are all synthesized in the brain or central nervous system and would not be possible without the enzyme tyrosine hydroxylase (2). An enzyme speeds up a reaction so it can occur in the time the body needs it to (2). In this case, the enzyme tyrosine hydroxylase speeds the synthesis of catecholamines (2).
Now, you may be wondering what exactly these neurotransmitters do for the gut aside from communication to the brain. Dopamine is the major catecholamine responsible for gut homeostasis (meaning it keeps the gut in the state it needs to be in to properly function) (2). Imagine it being your thermostat in your home. If you set the temperature to 72 degrees, it will do everything in its power to adjust its settings to maintain that temperature. So, if you open the door on a cold day and let freezing air in, the thermostat will turn on and produce more heat. This is what dopamine does for the gut; it keeps its environment at a specific “setting” and adjusts itself accordingly. Dopamine has been known to impact the absorption of electrolytes, like potassium and sodium, as well as protecting the mucosal layers from ulcers (2). It is also involved in gastric emptying which is the amount of time it takes for food to empty out of your stomach so it does not flood the intestines but it also does not sit in your stomach for too long (2).
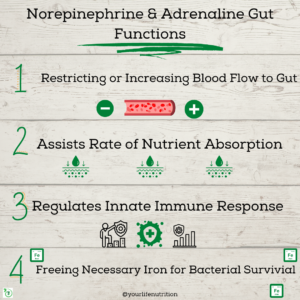
As mentioned previously, norepinephrine and epinephrine are the body’s “fight or flight” response. What exactly does this mean? These substances are elevated when the body is in a state of stress. For example, say you are walking in the neighborhood and suddenly a protective dog gets off of its leash and begins to run at you. Most often, the instinct is to run away from the impending threat. How would you accomplish this? Well, this state of “alert” increases your body’s norepinephrine and adrenaline because in order to run at a quickened pace, your heart needs more blood as it beats faster. Your muscles also need more oxygen (which you get from the blood) to accelerate. These catecholamines are involved in blood flow in the intestines by manipulating the blood vessels (2). When more blood is needed (like when you are being chased by a dog), epinephrine opens the blood vessels and when less is needed (like when you find safety and stop running) norepinephrine (as well as dopamine) constricts the blood vessel and overall flow back to normal (2).
They both also change the rate of nutrient absorption in the intestines depending on the body’s needs (2). The gut also has its own innate immune system to protect it from foreign pathogens (2). When something like a harmful bacteria gets into your system, the body attacks it which causes inflammation. Norepinephrine plays a role in mitigating the proinflammatory response as your body destroys these foreign substances so the entire body does not go into an inflammatory state (2). These catecholamines also aid in freeing iron necessary for bacterial survival in the gut and in regulating gut motility or the movement of the intestinal muscles for digesting food (2).
This may seem like a lot of information to process, so let’s review the key points. Your gut contains a microbiome of healthy gut bacteria that are involved in regulating mood, behavior, and cognition. There are chemical messengers called neurotransmitters that play an important role in communication between the gut and the brain. There are 5 neurotransmitters that all have an amine group (think amino acid or building block of protein) and carry out important functions impacting your gut and as a result your brain function. The first is serotonin, which was discussed in a previous blog. There are three catecholamines including norepinephrine, epinephrine, and dopamine. Together, these impact blood flow, gut motility, nutrient absorption, gastrointestinal innate immune response, and the microbiome population and health. The final biogenic amine group is histamine which we will discuss in another blog.
One major finding that we haven’t talked about yet is these neurotransmitter’s role in preventing disease. Studies have shown irregular levels of these substances to increase the development of diseases like Parkinson’s, autism, Irritable Bowel Disease, autoimmune diseases like Crohn’s and ulcerative colitis, and several other mood and behavior disorders (2).
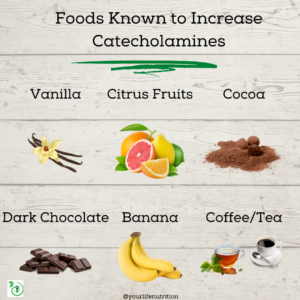
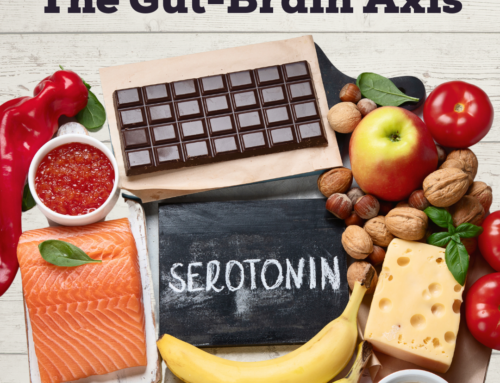
Believe it or not, there are some ways that you can help increase the level of catecholamine neurotransmitters. Here is a list of things to eat and activities to help (3):
- Coffee
- Tea
- Banana
- Dark Chocolate (aim for 70% or higher)
- Cocoa (unsweetened)
- Citrus Fruits
- Vanilla
- Exercise
- Stress Relieving activities
- Yoga
- Meditation
- Reading
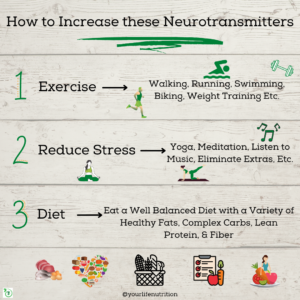
While reducing stress levels, exercise, and specific foods may impact the level of catecholamines in your body, the most important thing is to eat a well balanced diet and to stay active. This will help feed your microbiome and subsequently increase your neurotransmitters and gut health. Fiber is a big player in the microbiome, so eating lots of fruits with skin or pulp, veggies, and whole grains will help feed your microbiome and keep you happy, energized, and focused.
Post created by student dietetic intern from the University of Akron: Michaela Campbell
Works Cited
- Sudo N. Biogenic amines: Signals between commensal microbiota and Gut Physiology. Frontiers in endocrinology. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6685489/. Published July 31, 2019. Accessed March 30, 2022.
- Mittal R, Debs LH, Patel AP, et al. Neurotransmitters: The critical modulators regulating gut-brain axis. Journal of cellular physiology. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5772764/#:~:text=Neurotransmitters%20including%20serotonin%2C%20norepinephrine%2C%20epinephrine,et%20al.%2C%202009. Published September 2017. Accessed March 29, 2022.
- Catecholamine Blood Test. UCSF Benioff Children’s Hospitals. https://www.ucsfbenioffchildrens.org/medical-tests/catecholamine-blood-test. Published June 16, 2021. Accessed March 30, 2022.